- Home
- About
- Get P.A.D. Support Now
- Peripheral Artery Disease Info
- What is PAD?
- Join P.A.D. Support Groups
- Getting Tested for PAD
- What Causes PAD
- Find A P.A.D. Doctor
- Critical P.A.D. Bloodwork
- Eating With PAD
- Patient Conferences
- P.A.D. walking support program
- Medical NotePAD
- FootNotes
- PADdy's Post Newsletter
- Amputation Prevention Panel
- PAD Warrior Task Force
- PAD Awareness Ribbon
- Red Sock Day
- PAD: The Lived Experience
- The Heart of Innovation
- PAD Events
- Get Involved
- Swag Shop
- Donate
- 0

"My Steps" Sign-Up Here
Get daily accountability for every step you take via text!Let's do this!- How To Walk Handbook
A P.A.D. Warrior's guide to growing a "natural bypass" to reroute blood flow.
Highways And Detours
Walking As Medicine for PAD
How create your own 'natural bypass' to restore bloodflow to your feet.

When your physician says "Walking is the best medicine" for treating P.A.D., they're right. P.A.D. is defined by a narrowing of the arteries, mainly in the legs, due to plaque build-up. Plaque build-up causes arteries to narrow and lose their elasticity as they harden over time. That makes it difficult for blood to flow smoothly, if at all, to deliver critical nutrients, including oxygen to muscles, organs, and tissues. When flow is restricted, muscles, organs, and tissue are starved of critical nutrients, including oxygen. This may cause symptoms, such as leg pain and cramping when walking (claudication). Even worse, it could prevent healing of sores on your feet, leading to ischemia, meaning tissue loss. Wounds need oxygen to heal.
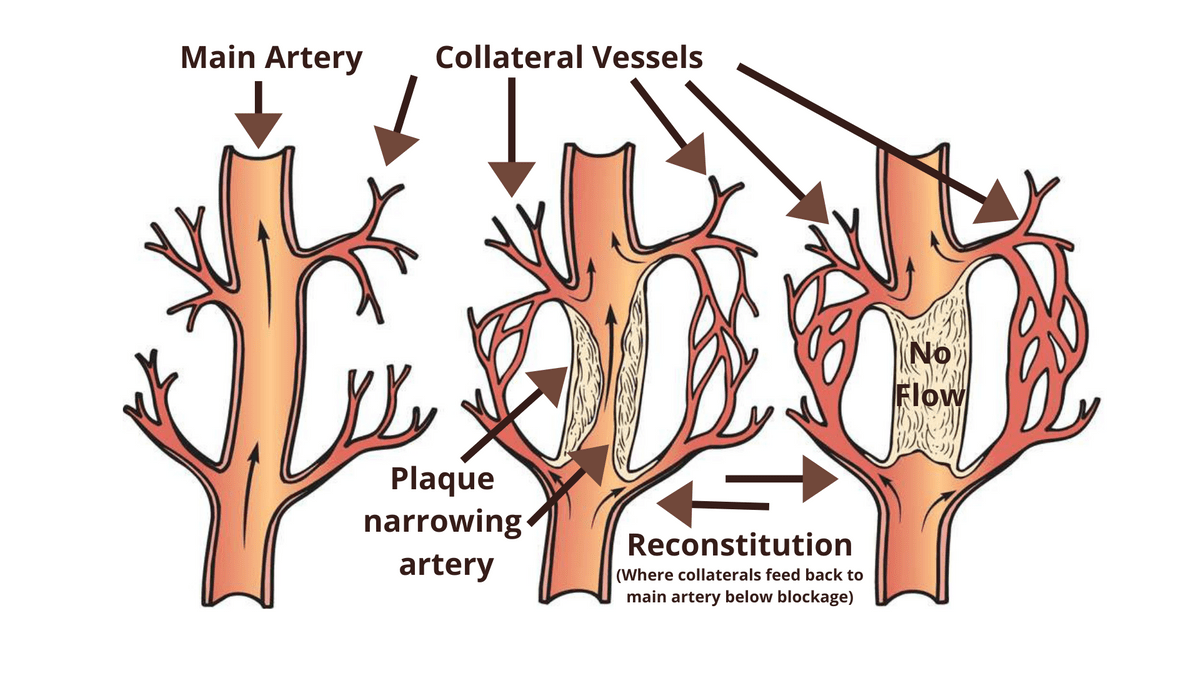
Your body does have a back-up system.
It's the collateral network, known as your body's "natural bypass."

The collateral network consists of smaller vessels available to handle extra demand. What makes them so special is they have the ability to expand and even grow if necessary to keep up with demand.
Walking helps to accelerate this process.
When you walk or exercise, your heart starts to pump harder and faster to circulate blood to deliver oxygen to your muscles, organs, and tissues. If arteries can't handle the additional rush of blood flow, the collateral vessels re-structure to meet the increased demand.

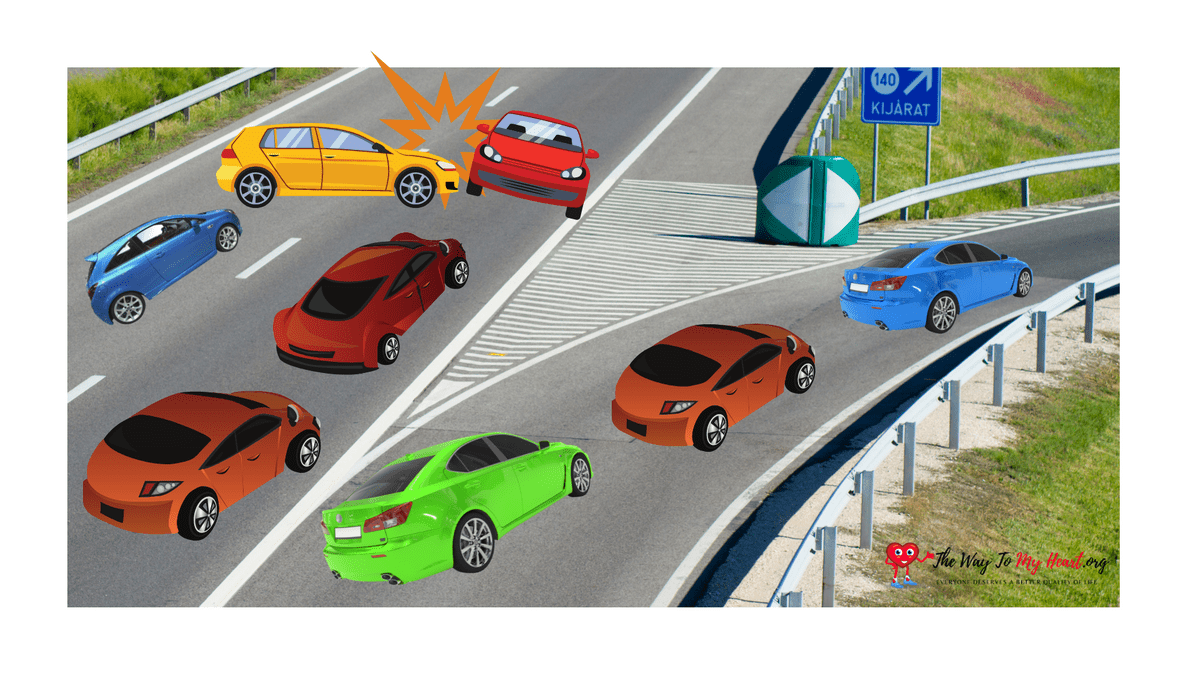
Think about it like our freeway system. If there's an obstacle such as an accident on the freeway blocking the flow of traffic, more cars veer off on to side roads to continue moving forward towards their destination. Collateral vessels, like side roads, can vary in capacity, but unlike side roads collateral vessels can expand and grow with increased demand. The extent to which your collateral network can keep up with demand, depends on the individual and stage of disease.
The collateral network's effectiveness may be limited in individuals with advanced age PAD and those with smaller vessel disease below-the-knee. That's why it's important to get a full vascular assessment. During this assessment, discuss with your physician:
- What is the extent to which you believe my body will be able to re-route flow and slow the progression of disease naturally?
- Based on my situation, what should be my daily and weekly walking goals?
- If walking is my initial treatment protocol, what symptoms are a warning for me to return prior to my scheduled follow-up for immediate re-assessment?
- What are next steps if my Ankle-Brachial Index (ABI) test improves by my next appointment?
- What are next steps if my ABI test does not improve by my next appointment?
For those without Critical Limb Threatening Ischemia (CLTI), standard protocols for treating P.A.D. suggest a three-month program that consists of medical and exercise therapy. During that time, physicians assess whether an antiplatelet drug and/or a vasodilator, coupled with brisk walking will help your body to increase flow not only through narrowed arteries, but also through the collateral network.
If you are post-procedure, following an intervention or bypass, your physician will prescribe a walking regimen to help maintain the recently treated vessels open, as well as to continue to maintain and build your collateral network. If a covered stent is used or bypass is performed collateral vessels will be impacted in those areas, but walking will remain critical to increase demand for blood flow to maintain those vessels open.
Beyond the initial formal walking program, ask your physician to continue to write walking prescriptions for The Way To My Heart’s My Steps program based on your individual needs and goals to increase long-term accountability.
- Read more about how to walk effectively to grow your natural bypass in the 20-page step-by-step PADdy's Post "Walking Special" handbook below!
- To learn more about our My Steps program and to participate in our monthly walking challenges which include prizes, sign-up below (Scroll down below PADdy's Post Walking Special.
- To find other P.A.D. Warriors walking to better health, join our FUN Facebook Walking Support Group here!
"My Steps" Sign-Up Here
Get daily accountability for every step you take via text!Let's do this!
The Way To My Heart © 2024